UNCOMMON HERO
The Tape That Rewrote Recovery

“There’s nothing more expensive than a failed surgery. If we can do it faster, stronger, better, why wouldn’t we?”
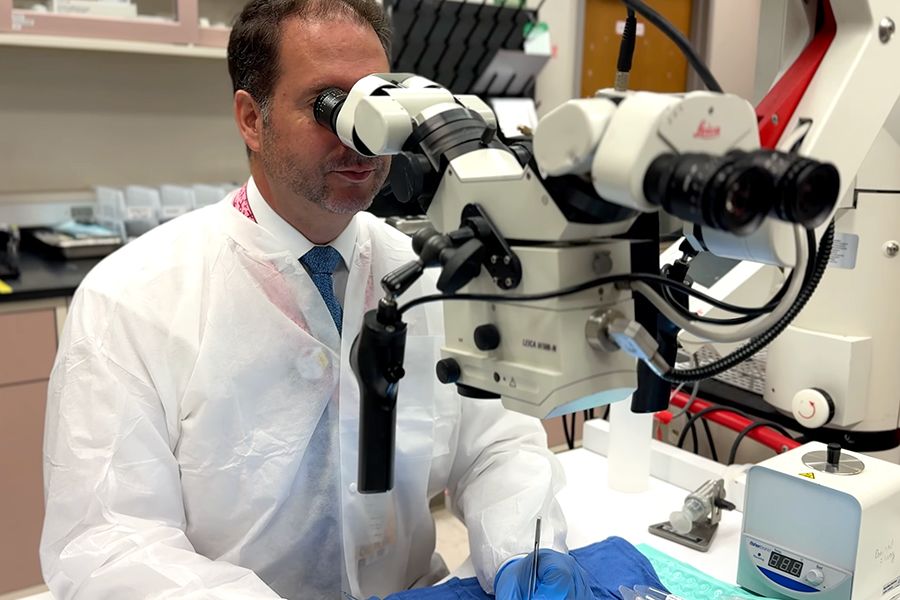
—Dr. Jonathan Isaacs, Chief, Division of Hand Surgery, VCU Health Department of Orthopaedic Surgery
Simple Idea, Global Breakthrough
Dr. Jonathan Isaacs didn’t set out to make surgical history. He just wanted to solve a maddening problem. For decades, even the most skilled surgeons repairing major peripheral nerves could only promise patients a 50-50 chance at full recovery — a coin flip at best. Backed by the unrelenting spirit of VCU, Isaacs decided to change that.
“Fifty percent. That’s been the reality for decades,” Isaacs says. “And that wasn’t good enough.”
Fifteen years ago, he began sketching ideas at his kitchen table, searching for a way to improve nerve repair. The early concept, a device to deliver healing compounds, fizzled. But one part stuck: the notion of joining severed nerve ends without sutures.
A blend of improvisation and persistence eventually led to a deceptively simple design: a flexible Scotch-tape-like band lined with ultra-small nitinol microhooks and a biological scaffold. It would become Nerve Tape.
The first prototypes weren’t elegant. Isaacs bought tiny fishing hooks, then later, delicate gold hooks from a fine jewelry designer at $10 apiece. “We’d drop half of them on the lab floor,” he laughs. “I told my assistant, ‘We might as well light $50 on fire and walk out.’”
Why Sutures Fall Short
For more than a century, the gold standard in nerve repair was suturing, a painstaking process of sewing minuscule, delicate nerve ends together. It was slow, technically demanding and often resulted in poor alignment, weakening recovery.
“Nerve Tape takes that step away entirely,” Isaacs says. “It’s simpler, faster and more precise.”
At VCU, Isaacs and his team demonstrated how the device could transform nerve repair. To show the broader surgical world, they invited outside institutions to test it, including Harvard’s Massachusetts General Hospital. The results were striking: Repairs with Nerve Tape were five times faster than sutures, with twice the strength and far better alignment. Even residents with limited experience achieved a 97% success rate, compared to 40% using traditional methods.
“In surgery, that’s a game changer,” Isaacs says. “It’s not just faster. It's better.”
Built the VCU Way
Isaacs is quick to point out that Nerve Tape might never have left the sketchpad without Virginia Commonwealth University.
“Other places told me to come back with $10,000 just to explore the idea,” he recalls. “VCU said, ‘Let’s build it.’”
From licensing to industry partnerships to funding, VCU smoothed the path from concept to commercialization. That support allowed Isaacs to work with a medical device partner, moving the idea into production and, ultimately, into operating rooms worldwide.
“It’s that VCU mentality,” Isaacs says. “We tackle what others can’t. Or won’t. And we do it fast.”
Unlimited Reach
Since its market debut, Nerve Tape has been used in more than 2,500 surgeries across a surprising range of specialties. Breast reconstructive surgeons were early adopters. The device added no time to complex operations and offered something invaluable: the chance to restore sensation.
Oral surgeons now use it in tight spaces where sutures are nearly impossible. Head and neck surgeons, long reluctant to reconstruct nerves after cancer resections, are beginning to change course. There are even early talks about adapting Nerve Tape to reinnervate the cornea.
One surgeon described it as “a small miracle in a sterile wrapper.”
Proof in the Numbers, Patience in the Process
Nerve regeneration is slow. It can take months or even years for outcomes to become clear. But so far, across thousands of cases, the device has had zero reported complications.
Isaacs and research teams at Mayo Clinic and the Hospital for Special Surgery are collecting long-term patient data while his VCU lab continues controlled studies to measure regeneration and muscle recovery.
“We’re confident in what we’re seeing,” Isaacs says. “Now we want others to validate it.”
Unmatched Impact
When asked what it means to see something so small — and born from something as ordinary as a fishing hook — change the future of surgery, Isaacs pauses.
“It’s humbling,” he says. “If this becomes the new standard, it won’t just improve surgery. It’ll improve lives.”
Then he smiles. “Besides, it’s the best fishing story I’ll ever tell.”
As a top 20% global university, Virginia Commonwealth University is an unparalleled powerhouse of innovation and creative problem solving. VCU attacks challenges as opportunities to do what others can’t. Or won’t. It’s truly a university unlike any you’ve ever seen.
This content was paid for and created by Virginia Commonwealth University. The editorial staff of The Chronicle had no role in its preparation. Find out more about paid content.