High-speed evolution: Tracking COVID variants in real-time

A year since its emergence, SARS-CoV-2 is producing new variants that influence its transmissibility and ability to evade immune response, forcing public health agencies and vaccine developers to adapt in step. Research at the University of Birmingham is playing a critical role helping keep pace with a fearsome foe.
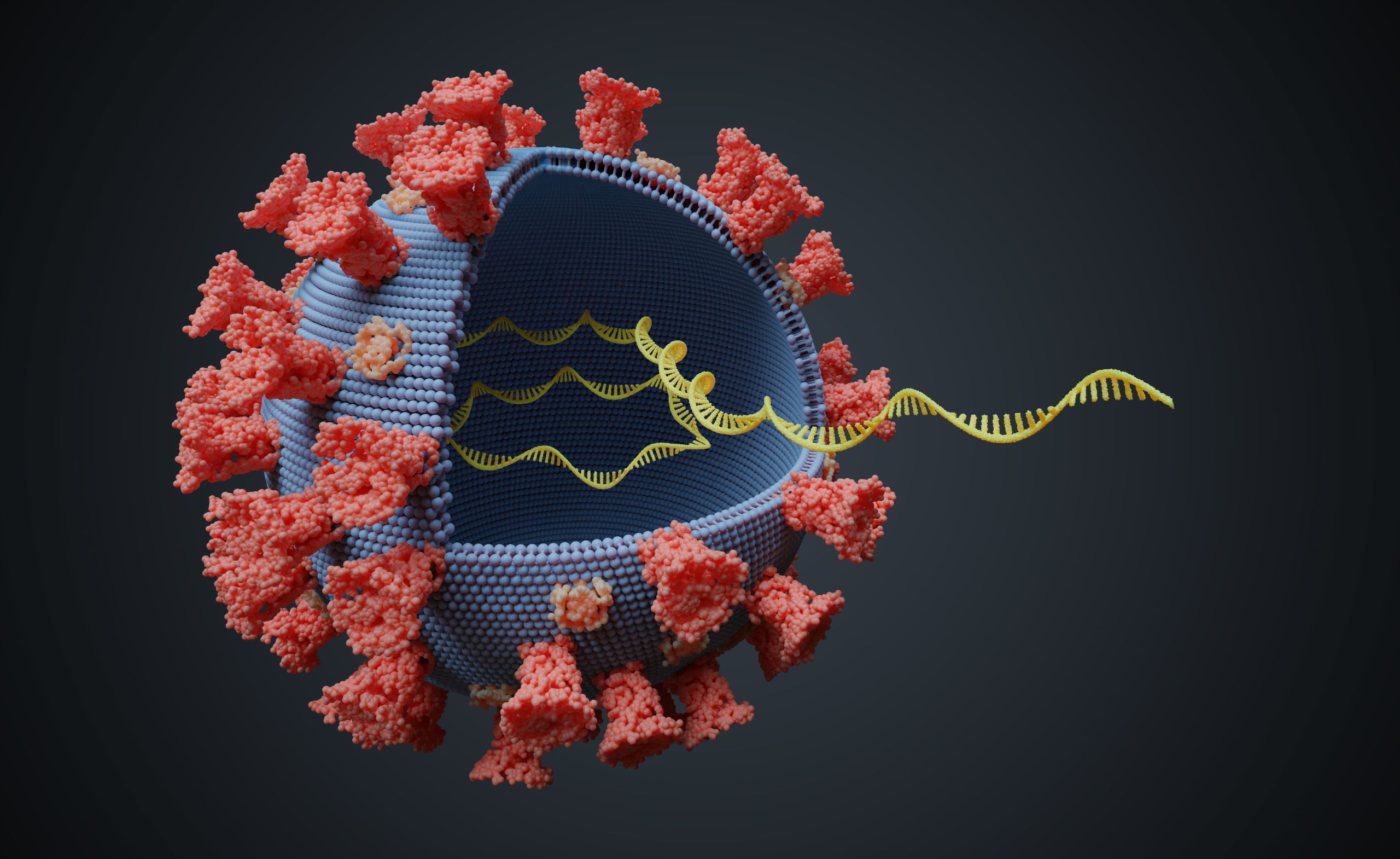
SARS-Cov-2 is one of seven types of coronavirus to infect humans, but its staggering global spread and death toll - now well over 2 million - shows that is it far superior to its predecessors, such as MERS and SARS, at passing between people and overwhelming human immune defenses.
More troubling is the fact that, the longer it rages, the more time it has to adapt and change.
Viruses are evolution in warp speed. They naturally mutate around twice per month, when small errors occur during the copying of genetic code during replication. Over time, some of these random mutations change the functioning of the virus in ways that can increase its ability to transmit between human hosts, outwit immune defenses, or both (just as other mutations make it less functionally efficient).
Understanding its mutations as they happen was, until recently, impossible. Now, thanks to advances in sequencing technology, the possibility of real-time genomic surveillance is here and is already guiding public health decision-making and vaccine development.

[WRAP-RIGHT]
[WRAP-RIGHT]
Nick Loman, Professor of Microbial Genomics and Bioinformatics in the Institute for Microbiology and Infection at the University of Birmingham, was working on techniques to track viral evolution before COVID-19. From 2014, he worked with the Oxford Nanopore platform, a new generation of portable genomic sequencers that revolutionized infectious disease surveillance.
“Previously, it took a long time to get genome sequencers and analyze viruses, so you were essentially looking at an epidemic retrospectively,” says Loman.
This Oxford Nanopore platform was cheap and portable “so we realized it was possible to do real-time genetic epidemiology where you can act quickly enough to influence how an epidemic unfolds.” Loman and his team worked on the Ebola and Zika outbreaks in West Africa and Brazil respectively.
When COVID emerged from China, Loman’s team was well-positioned to use the new tools and techniques to understand what this new disease looked like. Backed by funding from the Wellcome Trust to build new techniques for epidemic research, and with access to CLIMB, a farm of servers enabling the cloud-based big data analysis required for high-frequency genome sequencing, Loman and his colleagues played a pivotal role from the start.
Dr. Josh Quick, then a post-doctoral researcher, built a sequencing protocol within around two weeks of the first genome data released from China. Today, the majority of SARS-CoV-2 sequencing are using this protocol (UK research institutions as a whole have sequenced 250,000 genomes, around half the global total, using the protocols). “This showed how open source, open data methods really influence the course of the epidemic,” says Loman.
The second wave
Genomic epidemiology was initially helpful in understanding, with high precision, when cases emerged. The first wave of UK cases can be traced to an estimated 1,300 individuals travelling from Europe, primarily Italy, France and Spain.
During the summer, when overall infections were quite low, the technique helped researchers pinpoint ‘outbreaks within outbreaks’, such as a sudden spread in a hospital ward, workplace, or prison, which reveals sites where infection control measures were inadequate. However, when cases began to build again from September, monitoring took on a much more significant importance as the virus acquired dangerous new capabilities.
A new genomic lineage emerged in the south east of England, known as the Kent variant, and quickly dominated the overall caseload in a way that suggested it was far more transmissible. “Usually, you see hundreds of genomic lineages in any given location, but we saw that half of cases were coming from a single lineage, which meant one variant was taking off and growing faster than all the others,” recalls Loman.
“It also had an unusually high number of mutations. We would expect to see a lineage with 24 mutations after a year of circulating, but this one had 35, all in an area of the virus which determines how it gets into human cells.”
This became the Kent variant, or B.1.1.7. Loman’s team announced the finding which soon led to a change in UK government policy; a planned loosening of restrictions over Christmas was cancelled.
Two other variants, from South Africa and Brazil, are now also influencing travel and lockdown policies and even vaccine research.
“The virus has found multiple evolutionary paths to the same phenotype. Both are concerning because of their ability to evade immune responses, even in people who already had other forms of COVID previously."

“It has evolved to evade the immune response, which could affect existing immunity,” according to blood plasma analysis.
“This could mean re-infection and has implications for vaccine immune response because our current vaccines were developed based on the first version of the virus. The vaccines won’t be rendered useless, but this will have an impact on efficacy, so they will need to be reformulated as time goes on,” predicts Loman. The UK government has introduced surge testing in parts of England to understand exactly how much headway the South African variant has made.
For Loman, the experience of the last year has gone far beyond what he and his team anticipated when they first started studying the novel coronavirus. “This was conceived as a science project to explore viral evolution. You take a virus that has never seen a human body before and suddenly exposed to millions of human hosts, and you know it is going to be a big evolutionary experiment. But we did not think about how it might impact individuals or epidemic control."
This content was paid for and created by the University of Birmingham. The editorial staff of The Chronicle had no role in its preparation. Find out more about paid content.